Introduction: Understanding the Language of Pain in Dentistry
Dental pain is not just a discomfort, it's a diagnostic signal. According to recent studies, over 28–55% of people report experiencing tooth pain in the past 6 months, making it a critical symptom for early intervention in dental practice.
This guide helps dental students and professionals interpret the types of dental pain from a clinical lens and understand how pain patterns relate to specific oral pathologies. Whether it’s sharp, dull, or throbbing tooth pain, every sensation has a story to tell.
Jaiswal AK, Pachava S. Dental pain and self-care: a cross-sectional study of people with low socio-economic status residing in rural India. Int Dent J. 2015;65(5):256–260. doi:10.1111/idj.12175
1. Sharp Tooth Pain
"A warning signal of localised pathology"
This type of tooth pain is usually sudden, intense, and localised. Patients often describe it as a "jolt" or an "electric shock" sensation when they chew or bite down.
Common Triggers:
-
Carious lesions breaching the enamel and dentin
-
Cracked tooth or cusp fracture
-
Dentin hypersensitivity
-
Dislodged or loose temporary dental filling
Treatment:
-
Restoration (composite or GIC) using a quality dental composite kit
-
Crown placement for cracked teeth
-
Desensitising agents or varnishes
-
Root Canal Treatment
Clinical Tip: Sharp tooth pain often indicates compromised enamel or dentin exposure. X-rays, careful transillumination, or bite tests may be needed to localise cracked cusps or hidden carious lesions. These techniques rely heavily on advanced dental equipment for accuracy.
2. Throbbing Tooth Pain
"A classic sign of pulpal inflammation or infection"
This type of dental pain is characterised by deep, rhythmic, and persistent sensations—often described by patients as "pounding" or "beating." It can worsen when lying down and may radiate to the jaw, ear, head, or neck.
Likely Pathologies:
-
Irreversible pulpitis
-
Periapical abscess
-
Acute apical periodontitis
-
Necrotic pulp leading to infection
Clinical Management:
-
Pulp vitality testing and periapical radiographs
-
Root canal treatment with precision using endo rotary files or endodontic files
-
Antibiotics for swelling or systemic symptoms
Note: Do not ignore throbbing tooth pain even if it subsides—it often indicates an active infection.
3. Sensitivity to Temperature or Pressure
"Mild but persistent discomfort with cold, hot, or sweet stimuli"
This form of pain is transient but recurring. It occurs when stimuli (such as cold air, sugar, or touch) reach exposed dentine or irritated pulp.
Common Causes:
-
Enamel erosion
-
Gingival recession
-
Overzealous brushing
-
Post-treatment sensitivity (after scaling or whitening)
Clinical Considerations:
-
Look for non-carious cervical lesions (NCCLs)
-
Apply fluoride varnish or dentine sealants.
-
Recommend desensitising toothpaste and brushing modifications.
4. Dull Pain
"Pain upon pressure—suggestive of structural compromise"
Dull pain is a low-intensity, poorly localized, and continuous ache that originates from deep tissue structures such as dental pulp, periodontal ligament, or surrounding bone.
Common causes:
-
Periodontitis or Gingivitis
-
Bruxism (Teeth clenching or grinding)
-
TMJ pain
Treatment:
-
Professional teeth cleaning
-
Bite guard (if bruxism is present)
-
Soft Diet, jaw exercises (in cases of TMJ pain)
5. Radiating or Referred Pain
"When it’s not a tooth causing the ache"
Pain may sometimes be perceived in the mouth even though the origin lies elsewhere. This is known as referred pain and is especially challenging to diagnose.
Examples:
-
Myofascial pain of the masticatory muscles
-
Trigeminal neuralgia or neuropathic conditions
-
Cardiac origin (angina can radiate to the jaw)
What to Do:
-
Rule out local tooth pathology first
-
Refer for neurologic or systemic workup if the intraoral cause is excluded.
Recommended Read: Learn everything about Wisdom Teeth Removal Recovery Plan.
Prevalence and Self-Care Data in India
A landmark study conducted in Andhra Pradesh (ScienceDirect, 2020) found that 28.3% of rural residents reported dental pain in a 6-month period.
-
53.4% of them used OTC medication
-
11.9% applied balm or warm compress
-
Only 22.4% visited a dental professional.
Clinical Insight: Dentists must proactively educate patients about the importance of professional diagnosis over self-care alone.
Jaiswal AK, Pachava S, Sanikommu S, Rawlani SS, Pydi S, Ghanta B. Dental pain and self-care: a cross-sectional study of people with low socio-economic status residing in rural India. Int Dent J. 2015;65(5):256-260.
Comparison Table: Clinical Types of Tooth Pain
|
Pain Type |
Description |
Likely Cause |
Treatment Options |
|
Sharp Pain |
Quick, stabbing, often on chewing |
Decay, crack, loose filling |
Restoration, RCT, crown |
|
Throbbing Pain |
Rhythmic, pulsating, constant |
Pulpitis, abscess |
RCT, antibiotics, extraction |
|
Sensitivity |
Short-lived twinge on stimuli |
Recession, erosion, whitening |
Fluoride, desensitisers, varnish |
|
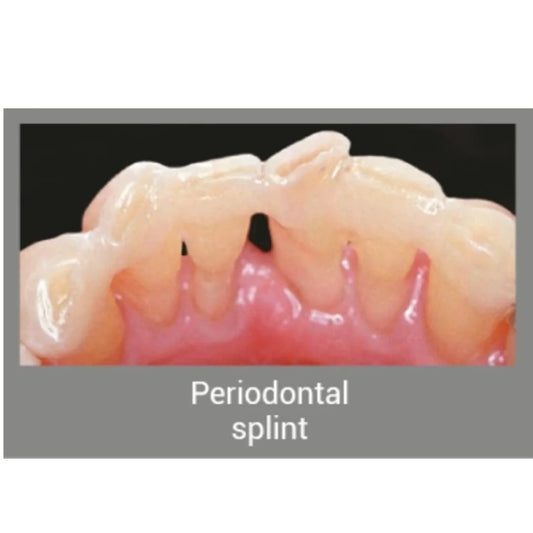
Pain While Biting |
Discomfort on occlusal contact |
Crack, trauma, high restoration |
Adjustment, splinting, endo |
|
Dull Pain |
Deep ache in tissue structures such as the dental pulp, periodontal ligament, or surrounding bone |
Periodontitis or gingivitis, bruxism (teeth clenching or grinding), and TMJ pain |
Teeth cleaning, bite guard (if bruxism is present), soft diet, and jaw exercises (in cases of TMJ pain) |
|
Referred Pain |
Radiates to the jaw or ear |
Neurological or systemic source |
Referral, interdisciplinary work-up |
Types of Dental Pain: Reversible vs Irreversible Pulpitis
|
TYPE of Pulpal pain |
Reversible Pulpitis |
Irreversible Pulpitis |
|
Definition |
Mild inflammation of the pulp due to irritation |
Severe inflammation, often a progression from reversible pulpitis |
|
Etiology |
Bacterial, chemical, or physical irritation (e.g., caries encroaching pulp) |
Usually follows untreated reversible pulpitis; deep caries, trauma, repeated irritation |
|
Pain Stimulus |
Thermal (hot/cold) or sweet |
Thermal (hot/cold) |
|
Pain Characteristics |
No spontaneous pain; |
Severe, persistent |
|
Localization of Pain |
Well localized |
Poorly localized; may radiate to ear, temple, eye, neck |
|
Nerve fibers <Cohen’s Pathways of the Pulp, 11th Edition> |
reversible pulpitis stimulates A-delta fibers (sharp, localized pain),) |
whereas irreversible pulpitis involves C fibers (dull, diffuse, often referred pain> |
|
Histologic changes in pulp <Hargreaves KM, Berman LH. Cohen’s Pathways of the Pulp, 11th ed. |
- Mild inflammation |
Intense, chronic inflammation |
|
Radiographic Signs |
None expected |
May show no early changes; late stages may show periapical inflammation |
|
Progression |
Can heal if the irritant is removed (e.g., filling carious lesion) |
Progresses to pulp necrosis if untreated |
|
Diagnostic Importance of Pain History |
Crucial for confirming pulp involvement |
Critical; helps determine if pulpitis is reversible or irreversible |
|
Diagnostic Tests |
Cold test: positive |
Cold & heat tests: lingering pain |
|
Palpation & Percussion |
Normal |
May be positive if periapical tissues are involved in later stages |
|
Management |
Address cause, monitor pulp recovery |
Depend on x-ray and clinical symptoms mostly Root canal therapy needed |
Final Thoughts for Dental Professionals
Understanding the types of pain in dentistry is crucial for both early detection and effective treatment. Remember:
-
Never ignore any form of tooth pain or toothache
-
Pain patterns give valuable clues to listen to your patient’s description.
-
Use diagnostic aids and evidence-based tools.
-
Educate patients to avoid dangerous self-remedies like tobacco, lime, or alcohol for pain relief.
For dental students: Always correlate symptoms with clinical signs and never treat based solely on the location of pain.
References & Sources:
-
Prevalence of Dental Pain and Self-Care – ScienceDirect
-
Tooth Pain Patterns and Etiology – ResearchGate
-
PubMed Search – Dental Pain in Rural India
Frequently Asked Questions (FAQs)
- Sharp tooth pain: Usually triggered by biting; could mean a cracked tooth or early decay.
- Throbbing tooth pain: Persistent and pulsating often a sign of infection.
- Tooth pain while eating: Sensitivity to pressure or temperature changes suggests decay or exposed dentin.
Each has unique clinical signs and requires specific dental evaluation.
But seek a dentist if you experience:
- Throbbing pain that disrupts sleep
- Pain that lasts beyond 2–3 days
- Teeth pain problems accompanied by swelling or fever Persistent or worsening symptoms often indicate an underlying issue that requires immediate attention.
This type of pain often stems from:
- Micro-cracks in enamel
- Failing restorations
- Loose fillings or crowns
It may not always be visible on X-rays, so your dentist may use a bite test or dye application to locate the source.
- Spread of infection to facial spaces
- Abscess formation
- Systemic issues like fever, fatigue, or sepsis in rare cases
Prompt diagnosis and treatment not only relieve pain but prevent long-term complications.
- Thermal and electric pulp tests
- Percussion and palpation
- Radiographs
To assess types of dental pain and identify whether it's reversible or requires endodontic or surgical intervention.