Dental procedures, and in particular, restorative and endodontic treatments often come with a range of post-operative complications such as pain, discomfort, post-operative sensitivity and even treatment failure. One of the major highlights is the development of reparative cement, designed to improve the success rate of various dental procedures by reducing complications. Reparative cements are versatile materials that are highly effective in creating biological seals, post-operative pain and faster healing. This blog delves into the role of reparative cement in resolving post-operative issues, the different types available and their uses in modern-day dental practice.
What are Reparative Cements?
Reparative cement refers to the group of dental cements and materials designed to encourage the tooth’s natural repair mechanism, by the promotion of hard tissue formation (encouraging the growth of new dentine) beneath the enamel in cases where the pulp is severely infected or irritated, even sealing off micro-leakages that could lead to post-operative complications, these materials not only restore the tooth structure but also to stimulate the biological repair process in the affected area.
Benefits of Using Reparative Cements in Dental Practice:
The main benefits of using Reparative Cements include:
Reduced post-operative sensitivity: It works by forming a protective layer over the exposed dentine, which helps in reducing the chances of pain caused by thermal or tactile stimuli.
Biocompatibility: Reparative cements are biocompatible with the surrounding tissues and tooth structures, thus minimizing the risk of inflammation and adverse reactions.
Promotion of tissue regeneration: Most reparative cements stimulate the formation of dentinal tissues and help heal pulp tissues, promoting the biological repair of the tooth.
Long-term sealing: They effectively seal without risk of bacterial invasion, reducing the risk of infections and future complications.
Reduced risk of post-operative inflammation: It reduces the risk of inflammation as they are less irritating.
Types of Reparative Cements
Glass Ionomer Cements (GIC):
Glass ionomer cement is one of the most commonly used dental cement/ reparative cement in restorative and other dental procedures. GIC is known for its excellent adhesive and bonding properties and is permanent dental cement, it bonds well to both dentine and enamel. Glass ionomer fillings biocompatibility makes it an excellent choice for applications near pulp tissue, also it releases a good amount of fluoride which helps in preventing secondary caries and promotes re-mineralization.
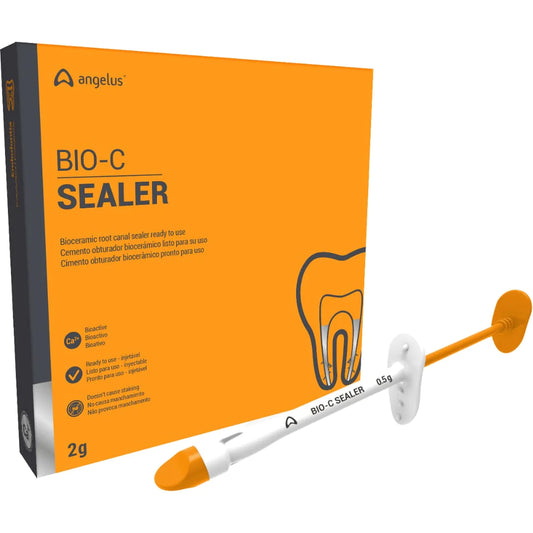
Mineral Trioxide Aggregate (MTA):
Mineral Trioxide Aggregate (MTA) is a bio-ceramic material widely used in endodontic and reparative procedures. it is well known for its ability to form hard, bioactive seals when it comes in contact with pulp and dentin. MTA is used for pulp capping, internal root resorption treatment, root canal therapy, and the creation of apical plugs during apexification. This material has high compressive strength which is ideal for restoring areas under mechanical stress.
Resin-Modified Glass Ionomers:
Resin Modified Glass Ionomer cement is an enhanced form of glass ionomer cement or dental cement, having both the features of glass ionomers and resins, offering superior bond strength and greater moisture resistance. Mainly used as fluoride-releasing materials for therapeutic (re-mineralizing) restorations and to create a bonding interface with good durability, also they are more aesthetically pleasing than conventional GIC.
Common Post-Operative Complications in Dentistry
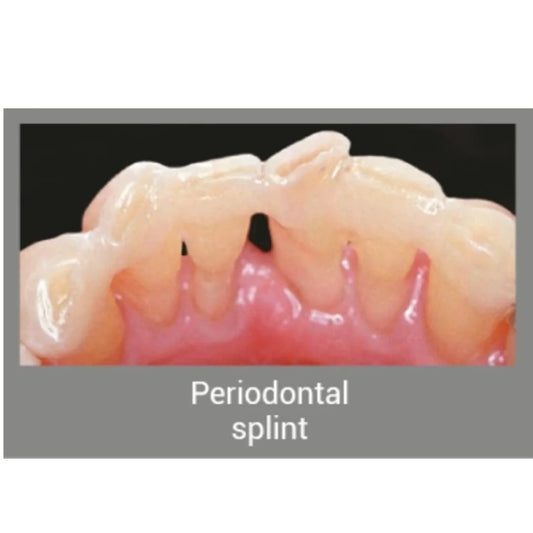
With the advancements in technology, dental procedures have become highly effective; post-operative complications such as sensitivity, pain, discomfort and infection are not uncommon. These issues arise due to the following reasons such as micro-leakage of restorations, irritation to the pulp or surrounding tissues and incomplete sealing. More often after root canal treatments, complications may arise and patients can experience:
Post-operative pain: due to the inflammation or infection in a particular area
Post-operative sensitivity: mainly caused due to exposure of dentinal tubules, which can lead to sensitivity to hot, cold or pressure.
Peri-apical abscess or pathology: if the sealing is not tight during the root canal process, bacterial invasion can lead to re-infection and require further intervention.
How Reparative Cements help prevent these complications:
Reparative cements can significantly reduce the chances of these complications:
Infection control: Cement and materials like calcium hydroxide have antimicrobial properties that can significantly reduce the risk of infection in the treated area.
Pulp protection: Materials like MTA help to protect the pulp from further damage by the formation of dentine bridge
Sealing of micro-leakages: This material effectively closes the micro gaps between the tooth and the material, preventing the ingress of bacteria that could cause infection.
Reduction in sensitivity: It helps reduce pain and discomfort by providing a hermetic seal over the exposed dentine area.
Conclusion:
Reparative cement plays a pivotal role in modern-day dentistry by reducing post-operative complications and helping in the promotion of long-term success of restorative and Endo procedures. by offering benefits like increased biocompatibility, good antimicrobial properties and tissue regeneration properties these materials can help save teeth from other interventions.
FAQs
Q. Can Reparative Cements Be Used in Every Endodontic Procedure?
Reparative cements can be used in endodontic procedures to seal and protect the root canal system. However, they cannot be considered for all endodontic procedures.
Q. How Do Reparative Cements Reduce Post-Operative Sensitivity?
Reparative cements help reduce sensitivity as they form a protective shield over the exposed dentine shielding the nerves from temperature and stimuli.
Q. What Is the Difference Between MTA and Glass Ionomer Cement?
The main difference lies in their properties and uses, as MTA is primarily used in endodontic procedures for its sealing abilities and promotion of pulpal regeneration, whereas GIC is permanent dental cement and is more used for restorative procedures because of its fluoride-releasing properties.